How To Write A Patient Discharge Summary
Learn how to write a patient discharge summary, what to include, and how to avoid common mistakes—plus download a free, ready-to-use template.

A well-written patient discharge summary plays a critical role in continuity of care. It ensures that primary care providers, specialists, and patients themselves understand what happened during hospitalization and what needs to happen next.
Whether you’re a clinician, hospital administrator, or healthcare organization standardizing documentation, knowing how to write a discharge summary correctly can reduce errors, improve outcomes, and save time.
In this guide, we’ll walk you through the process step by step, outline what to include, and show you how to create a discharge summary faster using a free, ready-to-use template.
What Is a Hospital Discharge Summary?
A hospital discharge summary is a clinical document prepared at the end of a patient’s hospital stay. It provides a concise but comprehensive overview of the patient’s admission, treatment, and discharge plan.
This document serves multiple purposes:
- Communicates essential information to the next healthcare provider
- Acts as part of the patient’s permanent medical record
- Supports continuity of care and follow-up treatment
- Helps meet regulatory, billing, and legal requirements
Because discharge summaries are often shared across care teams, clarity and completeness are essential.
When Is a Patient Discharge Summary Required?
A patient discharge summary is typically required when:
- A patient is discharged from inpatient care
- Care is transferred to another provider or facility
- Follow-up treatment or monitoring is necessary
Most healthcare organizations require discharge summaries to be completed within 24–48 hours of discharge to ensure timely communication and reduce gaps in care.

Essential Components of a Patient Discharge Summary
When creating a patient discharge summary, include the following core sections:
Patient Information
- Full name
- Date of birth
- Medical record number
Admission and Discharge Details
- Admission date
- Discharge date
- Admitting diagnosis
Reason for Hospitalization
- Chief complaint or presenting problem
- Relevant history leading to admission
Hospital Course and Treatment Summary
- Key findings
- Treatments provided
- Procedures or interventions performed
- Patient response to treatment
Consultations
- Specialists involved and their recommendations
Discharge Diagnosis
- Primary diagnosis
- Secondary or comorbid conditions
Medications at Discharge
- Updated medication list
- Dosage and instructions
- Changes from prior medications
Follow-Up Care Instructions
- Appointments
- Referrals
- Monitoring requirements
Pending Tests or Results
- Labs or imaging still awaiting results
- Who is responsible for follow-up
Patient Education and Instructions
- Lifestyle guidance
- Warning signs to watch for
- When to seek immediate care
Provider Signature
- Name
- Credentials
- Date completed
Including these elements ensures your hospital discharge summary is complete, compliant, and easy to understand.
Step-by-Step: How to Write a Patient Discharge Summary
Step 1: Gather All Relevant Clinical Information
Before writing, collect admission notes, progress notes, medication lists, lab results, and consultation reports. This prevents omissions and inconsistencies.
Step 2: Organize the Information Logically
Structure the summary chronologically—from admission to discharge. A clear flow makes it easier for the next provider to understand the patient’s care journey quickly.
Step 3: Write Clearly and Concisely
When writing a patient discharge summary, avoid unnecessary jargon or vague phrasing. Be precise, factual, and objective.
Step 4: Use Standardized Medical Terminology
Consistency in terminology reduces misinterpretation, especially when documents are shared across departments or facilities.
Step 5: Highlight Follow-Up and Next Steps
Follow-up instructions are one of the most critical parts of a discharge summary. Clearly state:
- Who the patient should see
- When should they follow up
- What actions are required
Step 6: Review for Accuracy and Completeness
Before finalizing, verify medication lists, diagnoses, and pending test details. Errors at discharge can lead to serious patient safety issues.
👉 Tip: Using a standardized template helps ensure nothing is missed.
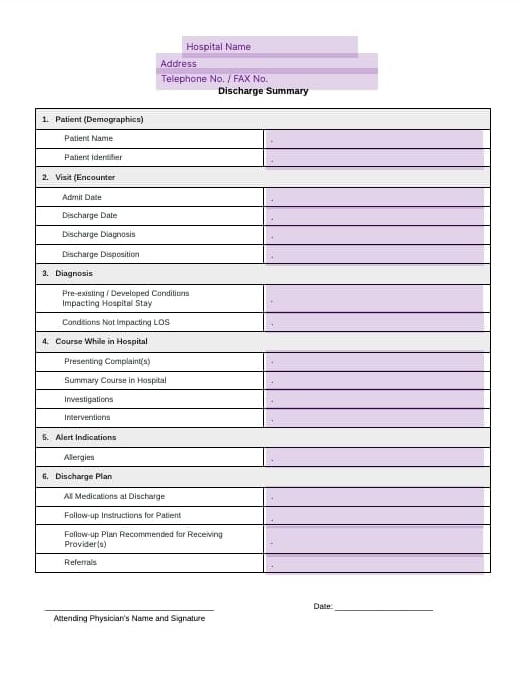
Download Our Free Patient Discharge Summary Template
Creating a complete and accurate hospital discharge summary doesn’t have to be time-consuming.
Our free patient discharge summary template is designed to help healthcare professionals:
- Follow a clear, standardized structure
- Ensure all essential sections are included
- Reduce documentation errors
- Save time during the discharge process
Use this template as-is or customize it to fit your organization’s workflow.
Common Mistakes to Avoid When Writing a Discharge Summary
Even experienced clinicians can make mistakes when documentation is rushed. Being aware of common pitfalls can improve the quality of a discharge summary and reduce post-discharge issues.
Missing or Unclear Follow-Up Instructions
Vague or incomplete follow-up guidance can lead to missed appointments and delayed care. Specify who, when, and what actions are required.
Incomplete Medication Reconciliation
Omitting discontinued medications, dosage changes, or new prescriptions increases the risk of errors. Ensure the medication list matches what the patient receives at discharge.
Delayed Completion
A discharge summary completed days after discharge can disrupt care coordination. Aim to finalize it within 24–48 hours.
Overly Long or Unstructured Narratives
Too much detail can hide key information. Prioritize clarity, highlighting diagnoses, medication changes, and follow-up plans.
Missing Pending Tests or Results
Failing to document outstanding labs or imaging can delay diagnoses. Clearly list pending tests and assign follow-up responsibility.
Avoiding these mistakes ensures safer care transitions, reduces administrative follow-ups, and makes your discharge summaries more effective.

Best Practices for Creating Effective Patient Discharge Summaries
Following best practices when writing a patient discharge summary helps ensure accuracy, compliance, and continuity of care—while also reducing time spent on revisions or follow-up clarifications.
Standardize the Format Across Your Organization
Using a consistent structure for every hospital discharge summary makes documentation easier to complete and easier to read. Standardization ensures that critical sections—such as discharge medications and follow-up instructions—are never overlooked, regardless of who prepares the summary.
Keep the Summary Clear and Action-Oriented
A discharge summary should focus on information the next provider needs to act on. Prioritize:
- Final diagnoses
- Medication changes
- Follow-up plans
- Red flags or warning signs
Avoid lengthy narratives that bury key instructions in unnecessary detail.
Write With the Next Provider in Mind
Remember that discharge summaries are often read by clinicians who were not involved in the patient’s hospitalization. Use clear medical terminology, avoid abbreviations that may be unfamiliar, and clearly explain any deviations from standard treatment.
Complete the Discharge Summary Promptly
Timeliness is critical. Best practice is to finalize the discharge summary within 24 to 48 hours of discharge. Delays can result in missed follow-ups, medication errors, and gaps in care coordination.
Verify Medication Reconciliation Carefully
Medication discrepancies are one of the most common sources of post-discharge complications. Always double-check:
- New prescriptions
- Discontinued medications
- Dosage changes
Ensure the medication list in the discharge summary matches what the patient receives upon discharge.
Use Templates to Reduce Errors and Save Time
One of the most effective ways to improve documentation quality is to use a structured template. Templates serve as built-in checklists, helping clinicians consistently create patient discharge summaries that meet clinical and administrative requirements—without starting from scratch each time.
Simplify Discharge Documentation With Fill's Ready-to-Use Template
Writing a discharge summary doesn’t have to be complicated or time-consuming. A clear, accurate patient discharge summary not only keeps your care coordinated but also helps prevent errors, improves communication between providers, and supports better patient outcomes.
With Fill, you can create discharge summaries faster and more consistently. Our ready-to-use template is designed specifically for busy clinicians, so you can focus on care—not paperwork.
👉 Download our free patient discharge summary template now and make discharge documentation simple, accurate, and stress-free.